Launching a pharmaceutical manufacturing company is a hard startup journey that involves lots of planning, regulatory compliance, technical setup, and strategic marketing. Our pharmaceutical startup guide will introduce you with everything from market research and business planning to obtaining licenses, setting up GMP-compliant facilities, and marketing your products. It covers the step-by-step process from planning to launch, including legal and regulatory requirements (local and international), essential licenses and certifications, equipment and clean-room setup, staffing needs, product types, financial planning and ROI, distribution channels, and quality-risk management. in this article we will cover “How to start a pharmaceutical manufacturing company,” “Pharma manufacturing setup,” “GMP and FDA certification for pharma,” “Pharma plant equipment list,” “How to get drug manufacturing license,” “Pharma business investment and ROI,” and “Marketing strategies for pharma startups” are highlighted throughout for online discoverability.

1. Business Planning and Market Research:
Below are a few important points to deal with Business Planning and Market Research:
Market Analysis: Firstly, identify unmet medical needs or therapeutic gaps. Research which drug products like (generics, branded, OTC, or specialty biologics) that are in demand in your target region. Next, analyze competitors, pricing, and regulatory landscapes. For instance, generics require knowing upcoming patent expirations, while biologics need biotech expertise. Consider also contract manufacturing (CMO) or PCD franchise models if full in-house production is initially too large-scale.
Business Model & Products: Will you manufacture small-molecule generics, branded innovator drugs, biosimilars, or niche products (e.g., injectables, ophthalmics)? Each type has different R&D and regulatory paths. Generics (chemical molecules) are identical to brands, while biosimilars are complex biologics “derived from living organisms”. You might start with a limited product line (e.g., tablets and capsules) and expand to syrups or injectables later.
Business Plan: Develop a detailed outline for products, including an analytics breakdown of the market, competition, pricing strategy, required investment in the pharma business, estimated ROI, and projected timelines. Alongside ROI estimates, draft the layout of your facility and processes for Pharma manufacturing, as well as your startup and ongoing cost projections. Within your projections, estimate ongoing costs which include wages, utilities, raw materials, and quality control, as well as startup costs such as land, buildings, and licensing. Research typical budgets, a modern GMP plant can cost millions of USD, depending on scale and product complexity.
Funding: Investigate options for securing funding. Traditional bank loans and equipment financing are commonplace. Venture capital or private equity may fund innovative biotech startups. Local drug manufacturing is subsidized in many countries, as it reduces reliance on imports, creating a granted incentive for domestic production. Given the global pharmaceutical market (~$1.27 trillion in 2020), governments often subsidize domestic production. Forming joint ventures with established pharma companies or offering contract-manufacturing services is another route.
Entity Formation: Choose a type of legal entity for your business (LLC, corporation, etc.) and register it in your region. Apply for general business permits and tax identification numbers. For all pharmaceutical licenses, this entity will hold the applications.
Facility and Infrastructure: Select a site that is compliant with regulations (safe environment, infrastructure, waste disposal system). Zoning for industrial chemical use may be required. Based on the subdivided operations (production, QA/QC labs, storing, and administration), design the facility layout annexed in Equipment. Hire specialized architects and engineers for GMP-compliant structures.
Recruitment: Define and expand your core team. Essential personnel include: Qualified Person (complying to UK/EU laws), leads for QA/QC, regulatory affairs, pharmaceutical engineers, seasoned production supervisors, and financial management. Early training in Good Manufacturing Practices (GMP) is vital. Under FDA regulations, a supervisor must be a fully trained employee who ensures the process is free from errors and contamination.
2. Legal & Regulatory Requirements
Pharmaceutical production is one of the most highly regulated industries. You must comply with both local drug laws and international standards:
Local Drug Regulations: In every country, there is a National Drug Regulatory Authority that gives out manufacturing licenses. In the USA, the FDA(CDER) regulates drug manufacturing, in Europe, the national agencies, or EMA (European Medicines Agency) set rules, and in India, the CDSCO (Central Drugs Standard Control Organization) grants drug licences. Do some research on your country’s drug laws early in your plans (e.g., US Food, Drug, and Cosmetic Act and 21 CFR Parts 210–211 for GMP fda.gov). Make sure your company/entity meets the criteria, as some countries need local ownership or partners.
Good Manufacturing Practice (GMP): Pharmaceutical quality is built on the foundation of GMP. It is not a “nice to have” certification; it’s a legal requirement across most jurisdictions. The World Health Organization defines GMP as “a system for ensuring that products are consistently produced and controlled according to established quality standards.” This applies to all production steps including raw materials and personnel training. The US FDA enforces cGMP (Current GMP) regulations which establishes minimum standards for facilities and processes to ensure product safety, appropriate strength, and identity. This means that your plant design, equipment, and operations must meet strict criteria of cleanroom classifications, validated processes, and batch records.
Many countries adopt WHO GMP guidelines or ICH (International Conference on Harmonisation) standards (e.g., ICH Q9 for Quality Risk Management, ICH Q10 for Pharmaceutical Quality Systems). Plan to implement a formal Quality Management System (QMS) and continuous improvement per ICH Q10.
Safety and Environment: Maintain occupational safety practices (fume hoods and ovens) and environmental policies (wastewater discharge, emissions of solvents). In some other countries, there are specific requirements, such as hazardous waste permits or disposal permits for effluents.
Import/Export Compliance: While planning for exportation, you must comply with the target countries’ regulations, like FDA registration for exports and EU batch testing. Access to some markets may require certifications as WHO GMP. On the other hand, imports of any raw materials or machinery are subject to customs and import control regulations.
Intellectual Property: Check that you own the rights to manufacture any of the drugs of your choice. Generic production of patented drugs is only allowed post-license or patent expiry. Innovator products would require patent rights or in-licensing for sales.
3. Required Licenses and Certifications
Starting production requires multiple specific licenses and approvals. Key ones include:
Manufacturing License: A drug manufacturing license (also called a pharmaceutical manufacturing authorization) is mandatory. For example, in the US, you must register your facility with the FDA within five days of starting operations and list all drug products. In India, a manufacturer must obtain a Drug License (Form 25/28) from the CDSCO after obtaining a state-level factory license. Manufacturing and Importation Authorization (MIA) is needed from the national medicines regulator (MHRA for the UK and ANSM for France) for France. These licenses certify that your site and processes meet GMP standards.
While compliance is needed for licensing, many regulators or customers may also require a formal GMP Certificate. WHO prequalification or certificate programs exist for export. Additionally, obtaining ISO quality certifications (e.g., ISO 9001 for QMS, ISO 13485 if making medical devices) can enhance credibility and marketability.
If producing certain categories, additional approvals are required. Controlled substances require a license from the DEA (US) or the relevant drug control authority. Special biological product licenses (FDA BLA and EMA centralized authorizations) are required for vaccines or blood products. Separate licenses may be needed under traditional medicine laws for Ayurvedic or herbal medicines.
These include effluent treatment, air emissions, and handling of hazardous wastes, which must be secured from environmental agencies.
In addition, registration for Goods and Services Tax (GST/VAT), import-export codes, and local business permits are mandatory.
Table: Key Regulatory Licenses and Issuing Authorities:
| License/Certification | Issuing Authority | Notes |
|---|---|---|
| Drug Manufacturing License | FDA (USA) / CDSCO (India) / EMA/NDRA | Legal permit to produce drugs; application includes plant inspection. |
| FDA Facility Registration | U.S. FDA (CDER) | Required for any US-marketed drug; facility registration and drug listing. |
| EU Manufacturing Authorization (MA/MIA) | National EU Medicines Agency (e.g., MHRA) | Permits manufacture/import in EU; includes Qualified Person oversight. |
| WHO GMP Certification | World Health Organization | Voluntary certification for international trade, based on WHO GMP guidelines. |
| Product Marketing Authorization | FDA/EMA/National Agency | Required before selling drugs; includes GMP inspection review. |
| ISO 9001 / ISO 13485 | International Organization for Standardization | Not mandatory, but signals quality; often required by buyers. |
| Controlled Substances Registration | DEA (USA) / National Drug Controller | Needed if handling narcotics/psychotropics; renewed annually. |
Every type of license comes with paperwork that needs to be filled out, Drafting the design of the facility, producing standard operating procedures (SOPs), and writing the quality manuals are examples of such documentation. Most of the time, there is an on-site inspection that needs to be done. As an example, to obtain a manufacturing license for a drug, you must first submit the floor plans of the building, the list of equipment to be used, the designated qualified personnel for the job, and the documented quality management systems/procedures. Inspectors will check if you’ve implemented the requirements of the documents before awarding you the certificate. In most cases, we see that many business owners prefer to hire regulatory consultants to help with these applications.
4. Facility and Equipment Setup (Pharma Plant Equipment List)
A GMP-compliant facility is critical. Key aspects include:
- Clean Room and Infrastructure: Design the Manufacturing Suites As Clean Rooms With Appropriate ISO Classifications, Such As ISO 8 Background For Non-Sterile Areas And ISO 7-5 For Sterile Production. Walls, floors, and ceilings must be smooth, impervious, and easily cleanable. Personnel air showers, gowning areas, and airlocks help prevent microbial ingress. For high-risk processes, unidirectional (laminar) airflow may be necessary. Positive pressure is maintained along with contaminant removal through HEPA filtration with Air Handler Units (AHUs). Sterile environments may require additional unidirectional airflow as described. Plans must include Clean Steam, purified water (WFI), and uninterrupted power supply. HVAC should control temperature and humidity for all products Waste treatment must comply with legal standards regarding solvent recycling and wastewater purification.
- Equipment for Production: Your production setup in Pharma manufacturing will differ according to the product. Some of the key equipment includes:
- Mixers and Reactors: Stainless steel vessels with blade-type agitators for liquid, suspension, and powder batch mixing.
- Filtration and Sterilization Systems: For clarification of solutions and removal of particulates, cartridge filters and vacuum deaerators are used. Equipment includes autoclaves, inline sterilizer’s and steam-in-place (SIP) systems for making sterile products.
- Filling & Packaging Lines:
- Liquid Filling Machines: Automated volumetric or peristaltic fillers for oral liquids, syringes, and injectables. For sterile products, monoblock or rotary aseptic fillers are needed.
- Solid dosage equipment: Tablet presses and capsule fillers (if manufacturing tablets/capsules) with dedusters. Pill coating machines, if required.
- Capping/Sealing: Induction sealers and ROPP or screw capping machines for tamper-evident sealed bottles. Crimping tubes fill for ointments and creams.
- Bottle Washing and Drying: Automated washing and drying equipment cleans containers before filling.
- Labeling and packing: Pack into final cartons using Label applicators, self-adhesive or sleeve, and cartoning. Traceability using barcode printers and vision systems.
- CIP/SIP Systems: Clean-In-Place and Steam-In-Place systems automate cleaning/sterilization of pipelines, tanks, and filters — essential for GMP compliance and quick batch turnover.
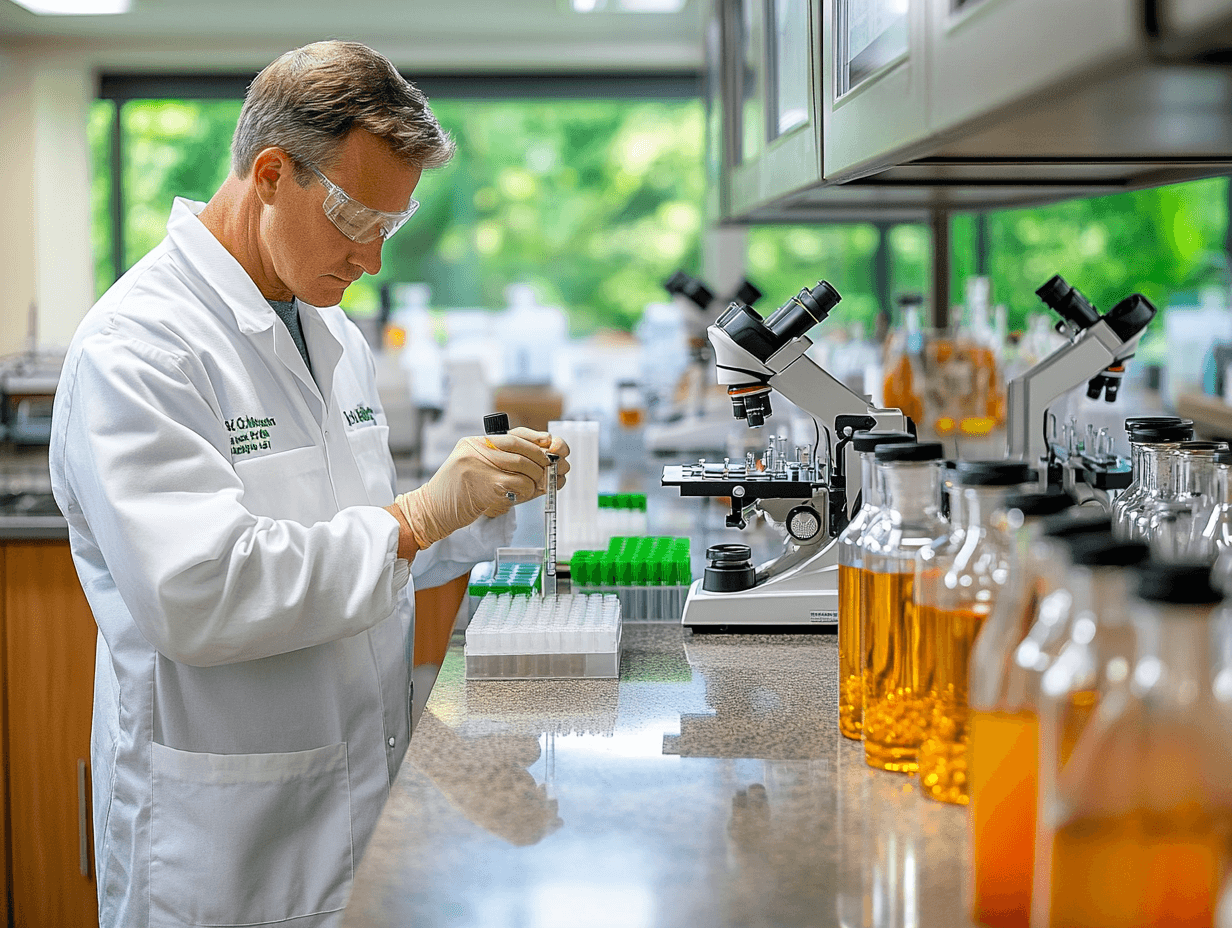
- Quality Control Laboratory: Different testing QC labs require specialized equipment such as HPLC/GC units, UV/Vis spectrophotometers, dissolution testers, microbial incubators, autoclaves, chemist microscopes, and titrators for moisture testing. The lab also has to have a balance, hardness testers, and incubators. Workflow and different analyses, like chemical vs microbiology, should be separated within the lab, and general laboratory practices within the industry have to be followed. For each raw material and the batches produced, trained analysts perform all of the necessary assays and confirm all processes through cross-check.
- Figure: Quality control laboratory layout – trained analysts conduct sample processing using an analytical microscope, balances in a controlled environment, while chemical reagents are incorporated. Establishing a fully-equipped QC lab is essential for GMP compliance and product quality.
- Support Utilities: Compressed air (oil-free), nitrogen (for blanketing sensitive products), purified water systems, and backup power generators also form part of the infrastructure.
When planning the Pharma plant equipment list, work closely with vendors. Many companies bundle turnkey solutions for specific dosage forms. Ensure all equipment is cGMP-compatible (e.g. sanitizable surfaces, validated controls). Obtain documentation like Operational Qualification (OQ) and Performance Qualification (PQ) protocols for validation.
Related:
List of Engineering & Utility Equipment
List of Quality Control Equipment in Pharmaceuticals
List of Pharma Equipment in Production Sections
5. Staffing and Human Resources
A successful pharma plant requires a multidisciplinary team:
Management and Administration: Operations are managed by a plant manager or a CEO. There is also staff assigned to manage business development, finance, budgeting, and accounts. HR is in charge of hiring, recruitment, and training.
Production Staff: Operators, mechanics, and technicians are trained in SOPs and GMPs. Special training is required for supervising personnel at larger plants.
Quality Assurance (QA): QA officers and managers are responsible for the QMS. They are in charge of batch record review, deviation management, change control supervision, and ensuring proper documentation. Under FDA CGMP, “persons who are qualified and fully trained” must be in charge of the manufacturing processes. A typical QA department allocates roles in documentation, process validation, and audits.
Quality Control (QC): Testing is performed by analytical chemists and microbiologists. Graduates in pharmacy, chemistry, and biotechnology are qualified. For routine checks such as raw materials and batch release tests, ensure sufficient staffing.
Regulatory Affairs: Responsible experts prepare submissions to local and international agencies for licenses, registrations, and labeling approvals. Knowledge of the local and international regulations is critical, especially for export.
Engineering and Technical: Engineering maintenance staff, like mechanical, electrical, or automation engineers, safeguard the functional health of critical equipment. Validation engineers, along with process development scientists, focus on efficiency and reproducibility for all validated processes.
Optional Research and Development: An R&D team formulates and works to optimize new and existing brands to be published while conducting stability studies on their formulations.
Additional Positions: Staff overseeing the warehouse, logistics personnel related to material handling, and the safety officers, as well as support staff trained in GMP cleaning procedures.
All personnel must be trained regularly in GMP, safety, and job-specific skills. Document all training. For example, FDA 21 CFR 211.25 requires that employees have “education, training, and experience to perform their assigned functions” in the manufacturing of pharmaceuticals. Recruiting from local technical colleges and offering ongoing professional development can build a skilled workforce.
6. Types of Pharmaceuticals to Manufacture
Decide early what types of products you will make:
- Small-Molecule Generics: The most frequent strategy chosen. Start producing duplicates of brand-name drugs like tablets and capsules after patent expiration. Although generics differ from brand names in terms of R&D Bio-equivalence requirements, the recovery period is always lesser as compared to new drugs. They are often chemically straightforward to produce in bulk and tend to have streamlined processes.
- Branded Innovative Drugs: This includes creating new proprietary meds or known brands under license. Even though this path offers better returns upon finding success, it comes with high R&D and regulatory cost burdens.
- Injectables and Sterile Products: Requires specialized aseptic manufacturing lines and advanced clean rooms. Biologics like vaccines or monoclonal antibodies are examples of such biologics and necessitate stringent regulatory supervision along with cell culture facilities and cold-chain capabilities.
- OTC and Wellness Products: Over-the-counter (OTC) drugs lie on the boundary between medication and supplements. These have less stringent criteria, such as creating herbal or vitamin supplements which require compliance with Good Manufacturing Practice (GMP) but are less complex than the regulations drug manufacturers have to work with.
- APIs vs Formulations: Some companies begin by producing APIs and selling them to formulators, while others concentrate on finished dosage forms. Selling API production to other manufacturers tends to be less stringent in regulations (despite global purchasers fretting about GMP and ISO standards).
Every Category Has Different Licensing Paths. For example, biosimilars and vaccines are under more stringent approval processes. Assess your team’s technical capabilities: start with chemical generics if you do not have biotech skills. Ensure market demand is met, for instance, targeting chronic disease drugs that have high patient volumes or specialized niche medicines.
7. Financial Planning, Startup Costs, and Funding
Pharma manufacturing is capital-intensive. Key financial considerations:
- Capital Expenditures (CapEx): Startup costs include leasing land, constructing GMP-compliant buildings, and purchasing equipment for the facility. A small solid dosage manufacturing plant could cost several million USD, whereas a large sterile biologics facility can go upwards of hundreds of millions USD. Additional expenses should also be allocated for clean utilities like WFI, ventilation, heating, and air conditioning systems, quality labs, as well as for validation and commissioning processes.
- Working capital, along with operational expenses, includes stocking up raw materials, endorsing bulk inventory, especially when exporting, paying salaries, and adhering to GMP operation costs that heighten utility expenses for cleaning, HVAC, pure water, and compliance expenditures for quality monitoring tests and waste treatment.
- Break-even and ROI: Recovery of investments can take decades. Generic drug makers usually reach consistent margins that are optimized between 10-15%. Biosimilars and innovative drugs tend to take longer, but have the potential for much greater profit. Use conservative sales forecasts and look into contract-manufacturing partnerships to guarantee some revenue early on.
- Funding Options:
- Funding Options: Bank Loans/Equipment Financing: Obtained easily for large pieces of equipment. Mortgages on real estate or equipment leasing can improve cash flow.
- Equity Investment: Venture capital funds or strategic partners from pharma companies can finance in exchange for shares. Biotech has government venture funds in other regions.
- Government Grants/Subsidies: Some countries support local pharmaceutical companies with tax breaks or grants, as seen with “pharma parks” in India. Look for such programs in your country.
- Partnerships: Think about toll manufacturing or joint venture agreements with more established companies. This can help share both costs and risk.
- Insurance and Risk Mitigation: Insure the facility, equipment, and liability (product liability insurance). Plan for contingencies like equipment downtime or regulatory delays.
In financial planning, highlight the ROI potential, like the global demand for medications is growing, so a successful plant can be a regular income source over decades. Prepare detailed cost projections, funding plans, and sensitivity analyses for investors.
8. Distribution and Marketing Strategies
Develop strategies for getting your products to market:
a. Distribution Channels:
B2B Sales (Institutional): Most pharmaceuticals are sold through business channels. Forge relationships with drug distributors, hospital procurement departments, and government tenders. Attend industry trade shows and join professional associations. In many countries, sales reps or regional managers call on doctors and pharmacists to list products. For institutional accounts (hospitals, clinics), establish contracts or participate in bidding/tender processes.
Wholesale and Retail: Partner with national and local wholesalers who stock and supply pharmacies. Ensure your pricing and margins align with these intermediaries.
E-Commerce (for OTC): If manufacturing OTC medications or supplements, consider online sales platforms. Digital pharmacies and direct-to-patient models are growing, especially post-COVID.
b. Marketing and Branding:
- Wholesale and Retail: Collaborate with pharmacy suppliers and national or local wholesalers. Be sure to maintain proper pricing and margin structures with these wholesalers.
- E-Commerce (for OTC): Consider online sale opportunities if producing OTC medications or supplements. Digital pharmacies and direct-to-patient models are on the rise, especially in the post-COVID world.
- Establish a professional brand (generic or not, having a name people recognize helps) – construct packaging and labeling that has marketing clearance. Use content marketing and digital marketing to educate professionals about the product (SEO, social media).
- Use KOLs and conferences to showcase your brand credibility. Give medically accurate promotional material to physicians and patients about your products.
- For products targeting the end user, local regulations must be followed for drug advertising on television, print, and online. Many countries restrict marketing of prescription medicines directly to consumers. However, branding can be aided indirectly through disease awareness and educational campaigns aimed at patients.
c. Online Presence:
Maintain an informative website (a digital presence is now essential). Use SEO strategies – for example, optimizing for queries like “how to get a drug manufacturing license” or “GMP and FDA certification for pharma” – to attract entrepreneurs and customers alike.
d. B2B Marketing Tactics:
According to industry experts, targeting the right audience segments is crucial. These include healthcare providers, pharmacies, hospitals, and group purchasing organizations. Data analytics can identify prescribing trends. Multi-channel outreach (emails, webinars, scientific journals, LinkedIn) increases engagement. Positioning your firm as a reliable, quality-driven supplier with timely deliveries and strong technical support will differentiate you.
e. Regulatory Marketing:
Make sure all advertisement materials go through your regulatory team. Regulatory action can stem from misbranding or false claims. As a part of trust maintenance for your products, you need to implement pharmacovigilance: monitor and report adverse events as required.
In summary, marketing strategies for pharma startups should combine outreach to professionals (B2B), and, where applicable, safe messaging to consumers (B2C) while always highlighting compliance and GMP quality.
9. Risk Management and Quality Assurance
Maintaining product quality and managing risks is a continual obligation:
Quality Management System (QMS): Implement a robust QMS covering all operations. This includes Standard Operating Procedures (SOPs), document control, deviation handling, CAPA (Corrective and Preventive Actions), and internal audits. Many companies align with ICH Q10 (Pharmaceutical Quality System) and ISO standards. A dedicated QA department should sign off on every batch release.
Quality Risk Management (QRM): Focus on minimizing risk in a manufacturing process. FMEA, HACCP, and PHA are some tools presented in ICH Q9. For example, you can conduct an FMEA on a sterilization process to determine failure points so you can control them. The results of risk assessments must be documented for critical steps, e.g., sterile filtration.
Raw Material Control: Scrutinize suppliers of APIs and excipients. Issue CoA and audit important suppliers. Employ approved vendor lists alongside incoming inspection and testing. Inputs that are adulterated or substandard pose significant risks.
In-Process Controls: In production, check and monitor for temperature, pH, and weight. Implement validation for cleaning procedures to ensure no cross-contamination between batches.
Release Testing: Comprehensive QC testing must be done prior to the issuance of finished goods. Evaluate analytical procedures to confirm identity, potency, purity, and sterility (if applicable, for sterile products).
Audit and Inspection Readiness: Be prepared for regular inspections from regulators like FDA or CDSCO, and even by your clients. Preserved batch records, logbooks, and training logs should be up to date and accessible. Inspectors evaluate if the firm possesses the appropriate facilities and equipment, along with the technical capability to manufacture the drug. Violations can result in warning letters or business cessation.
Recall and Contingency Plans: Define your procedures for receiving product complaints and initiating recalls. Though such situations rarely arise, policies should outline how to trace, trap, and return defective items. Maintain standby strategies for critical instruments.
Continual Improvement: Command policies must address how continuously improving quality systems will be incorporated. Provide training on the latest quality standards to all employees, as GMP is constantly on the move. Hold management meetings and track metrics like OEE for effective continuous improvement.
You mitigate risks to patient safety, defend your brand, and manage safety while protecting corporate integrity by embedding quality (QA culture) into every process. Such processes aid the company in avoiding ‘adulterated’ outcomes, which would deem the company legally non-compliant, even if no visible discrepancies are detected.
Sources: Authoritative regulatory and industry references were used throughout, including FDA guidance on cGMP fda.govfda.gov, WHO GMP guidelines who.int, and industry reports wolterskluwer.com, corpseed.com, among others) to ensure accuracy on regulations, licensing, and best practices.
Naresh Bhakar is the Founder and Author at Pharmaguddu.com, bringing his extensive expertise in the field of pharmaceuticals to readers worldwide. He has experience in Pharma manufacturing and has worked with top Pharmaceuticals. He has rich knowledge and provides valuable insights and data through his articles and content on Pharmaguddu.com. For further inquiries or collaborations, please don’t hesitate to reach out via email at [email protected].